When Katie Spanos ’20 enrolled at Dartmouth as a biological sciences major, she was confident that her ultimate goal was a career in health care. But she wasn’t sure which role was best for her.
Spanos learned of the Nathan Smith Society—a Dartmouth student organization that organizes programming related to the health professions—and joined its Clinical Shadowing Program, which pairs students with health care professionals at Dartmouth Hitchcock Medical Center and private practices in the Hanover area.
During a placement with the critical care team at DHMC, Spanos found the perfect fit.
“I observed the entire health care team, including the lead physician, the physician’s assistant, a resident, and a nurse practitioner,” Spanos says. “Watching the team dynamics play out gave me the clarity I wanted. I knew then that I wanted the responsibilities of a physician: being a team leader, providing compassionate care, and engaging patients in important conversations about their health.”
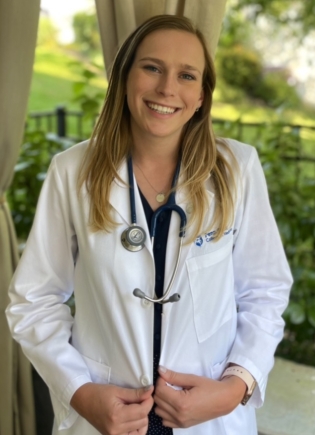
Now a third-year medical student at Penn State College of Medicine, Spanos leads research on eating disorder relapse prevention. She plans to continue her research during her career as a physician while spending the majority of her time in clinical settings.
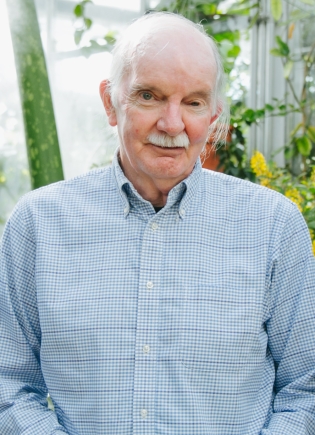
Spanos is one of more than 5,000 Dartmouth undergraduates who have gained firsthand insights about health care fields through the Clinical Shadowing Program since its inception in 1997. Founded by Professor Lee Witters, who holds a joint appointment with the Faculty of Arts and Sciences and the Geisel School of Medicine, the program celebrates its 25th anniversary this academic year.
“I wanted to give undergraduate students the opportunity to see what it’s like to be a physician, to hear the pros and cons of a life in medicine, and to determine if they are comfortable being around patients,” Witters says.
A retired endocrinologist, Witters is the only physician in the Department of Biological Sciences, and also serves as the Eugene W. Leonard 1921 Professor of Medicine at Geisel’s medical education and biochemistry and cell biology departments.
“Students are able to take advantage of a top academic medical center just minutes from campus, which provides access to over 100 doctors in almost every area of medicine. It’s one of the best undergraduate shadowing programs in the country,” Witters says.
Witters manages the program alongside a small team of Nathan Smith Society student leaders, who use a lottery system to ensure that shadowing experiences are evenly distributed. Each year, approximately 250 students participate in the program over the course of Dartmouth’s four academic terms.
“We have every variety of physician you could think of—general internist and primary care practitioners, surgeons, OB/GYN and midwives, pediatricians, anesthesiologists, neurologists, radiologists, radiation therapists, and even people involved in laboratory medicine—as well as nurses, nurse practitioners, and genetic counselors,” Witters says. “Even the DHMC chaplain is involved; he offers an incredible experience which allows students to see patients in a very different way than a physician would.”
Insider perspectives on health professions
For UCLA anesthesiology resident Christina Ma ’14, the program was her first chance to see what practicing medicine is really like.
“No one in my family was in the medical field, so simply being exposed to different practice environments and learning what it means to ‘round’ was highly informative,” Ma says.

Elijah Stommel, a DHMC neurologist and Geisel professor of neurology who has been part of the shadowing program since its inception, calls the experience a “mind opener.”
“Most undergraduates have no idea what clinical medicine is all about,” Stommel says. “I don’t expect them to learn much about medicine itself, but rather to get a feeling for what is involved in being a physician and what the experience of being sick is like for the patient.”
The program also offers opportunities to correct misconceptions that students may have about the field of medicine.
“One of the most striking things for many students is that there’s very little discussion about the surgical process in the operating room,” says John Sanders, a retired cardiac surgeon and Geisel professor emeritus of surgery, who has led shadowing experiences in the cardiac operating room since 1997.
“Movies and television shows often depict high drama in the operating room, but it’s just not that way. The actual conduct of the procedure is very calm, very quiet, and very orderly. For me, it was always a very peaceful place. I think it’s good for students to see that the operating room is not a scary environment.”
For Pulkit Nagpal ’23, observing in the operating room was a reminder that medicine—and especially surgery—is a team effort.

“From the outside, you kind of feel like a surgery is just about the surgeon doing his or her thing,” he says. “The reality is that the surgeon works with a team during every procedure. I had the opportunity to talk not only with the surgeon, but also with the other people involved, including the tech, the nurses, and the anesthesiologist.”
Many of the health care professionals involved in the program go out of their way to provide context, explain procedures, and make students feel included. For example, Sanders always starts shadowing experiences in the cardiac operating room in the same way: Breakfast, a brief history of heart surgery, and an overview of surgical technology.
“I always feed them before we enter the operating room—they’re much more likely to stay upright if I do,” Sanders says. “Then I usually go through the cardiac catheterization laboratory, where a lot of the diagnostic and therapeutic procedures are done, and show them some of the images that relate to the case that we will observe. I also describe the history of open heart surgery—a good deal of which I helped develop.”
Amalya Wilson ’23, who spent three days over the past summer shadowing pediatric orthopedic surgeon William McKinnon, says he consistently spent extra time contextualizing cases and explaining procedures.
“Before each appointment, Dr. McKinnon would pull up the patient’s X-rays and review their condition, prognosis, and relevant history with me so that I would understand the conversation,” Wilson says. “After the appointment, he encouraged me to ask questions and would answer my questions thoughtfully. When we were in the operating room, he made sure I had a clear view of the patient and understood the nature of each procedure, pausing frequently to explain his maneuvers.”
Nagpal also received a warm welcome while shadowing maxillofacial surgeon Eric Peter Holmgren.
“One of the coolest things I remember about shadowing Dr. Holmgren is being included in the timeout, which surgeons do at the beginning and end of every surgery to say who’s on the team and what they’re doing,” Nagpal says. “Dr. Holmgren invited me to participate in the timeout, so I got to say, ‘I’m Pulkit, I’m the shadowing student, and I’ll be observing today.’”

In fall 2022, Wilson shadowed Thomas Trimarco, an emergency medicine physician at DHMC. Despite the fast pace of the emergency department, Trimarco challenged Wilson to think like a physician by asking her to assess each patient’s condition.
“After we left each patient’s room, Dr. Trimarco would turn to me and ask, ‘Sick or not sick?’” she says. “I would then share my hypothesis, and he would respond with his thoughts. These short conversations provided me with much insight into how physicians think—what piques their concern, what alleviates worries, what they pay close attention to.”
Preparing future health care providers
Beyond revealing the realities of life as a physician, the shadowing program also enables students to hone valuable interpersonal skills.
“In the emergency department, I learned a lot about being present,” Spanos says. “It amazed me how the doctor would manage so many patients while also charting and communicating with nurses, radiology, and the lab. Even in the midst of all that chaos, he was very present with each patient and listened to their concerns without interruption or judgment.”
Nagpal also appreciated the reminder that practicing medicine requires both intellectual and emotional intelligence. “As an undergraduate pre-med student, you’re put into classes and you memorize a lot of stuff,” he says. “While it’s important to be book smart, being a good physician is really about the way you connect to patients.”
“The doctors I shadowed offered great examples of bedside manners,” he says. “Often, the patient came into the appointment nervous; the doctors could sense that and would make the small talk needed to calm them down. There’s a tone of voice and an empathy that you learn when you’re shadowing that you don’t really get to see in any other setting.”
Spanos also learned the value of emotional resilience and prioritizing her own mental health. “In critical care, I watched as the team managed the sickest of the sick and had extremely difficult conversations with loved ones,” she says. “I talked to the physician’s assistant about the emotional toll that providers experience, and we had an extremely real and valuable conversation about burnout and the importance of self-care in this field.”
For many students, participation in the shadowing program instills a passion for medicine that sustains them through the long journey of becoming a physician.
“It’s a long haul from the undergraduate level through medical school to residency,” Sanders says. “Shadowing gives students the sense that it really is worthwhile.”
“Activities like the shadowing program, along with volunteerism in a number of situations, are really what medical schools are seeking,” Witters says. “The shadowing experience provides lots of stories that students can tell in the essays and interviews that are part of the medical school application process. I would say, from my own experience on faculty at Geisel, that Dartmouth students who apply to medical school are very well received.”
The shadowing program helps students solidify their career goals—just as Spanos did.
“‘Going into medicine’ does not have to mean going to medical school,” Spanos says. “It’s important to figure out which role within the medical field is right for you. If you’re sure you want to be a physician, use this time as an undergraduate to feel out different specialties and start to develop your preferences.”
For Witters, watching students learn and discover their path makes the labor of administering the shadowing program worthwhile.
“I’ve now been around long enough to see the impact this has had,” Witters says. “The Clinical Shadowing Program has helped thousands of students get to where they want to be, whether they choose to go into medical professions or not. Seeing their maturation is incredibly rewarding.”
